When Australian cricketer Nic Maddinson discovered a lump and promptly reported it to his team doctor during a routine review in April 2025, he thought catching it early would be his safety net. Seven weeks later, he learned the devastating truth: despite immediate treatment, testicular cancer had already spread to his abdominal lymph nodes and lungs.
Maddinson, born in Nowra, New South Wales, made his international debut for Australia in a T20I at Rajkot, India in October 2013, scoring an impressive 34 off 16 balls. He went on to play three Test matches for Australia in 2016—all at home against South Africa and Pakistan—and six T20 internationals for his country. He also represented Royal Challengers Bengaluru in the Indian Premier League during 2014-2015, playing 3 matches and scoring 20 runs with a highest score of 12. In August 2016, Maddinson scored a century (118) for Australia A against India A at Mackay, a performance that thrust him into Test calculations and nearly earned him selection for the Border-Gavaskar series.
“To know that I caught it probably as early as I could have, and it still spread into other parts of my body, that was scary,” the 33-year-old revealed in a candid interview this week. His experience delivers a sobering message to the millions of young men worldwide at risk for this aggressive disease: early detection matters, but time matters even more.
The Young Man’s Cancer Most Don’t See Coming
Testicular cancer is the most common malignancy affecting males aged 15 to 35, accounting for approximately 5% of all urological cancers despite being rare overall. Globally, testicular cancer affects roughly 2.8 per 100,000 young men.
What makes this cancer particularly insidious is its stealth progression. Most men, like Maddinson, initially attribute vague symptoms to minor health issues—viral infections, fatigue, or general malaise. By the time a palpable lump appears, the cancer may already be advancing beyond the testicle itself.
Eight Warning Signs Every Man Should Know
Medical experts identify eight critical warning signs that demand immediate medical attention :
Primary symptoms (in the testicle):
- A painless lump or swelling in either testicle, potentially as small as a pea or marble
- Change in how a testicle feels or a sensation of heaviness in the scrotum
- Pain, discomfort, or numbness in a testicle or scrotum, with or without swelling
- Sudden buildup of fluid in the scrotum
Advanced symptoms (indicating possible spread):
- Lower back pain, shortness of breath, or chest pain
- Persistent cough or bloody sputum
- Dull ache in the lower abdomen or groin
- Unexplained fatigue or significant weight loss
Maddinson experienced several of these symptoms before his diagnosis. He felt persistently rundown, attributed it to a viral infection, and only mentioned the lump during a routine team medical review. That casual mention likely saved his life.
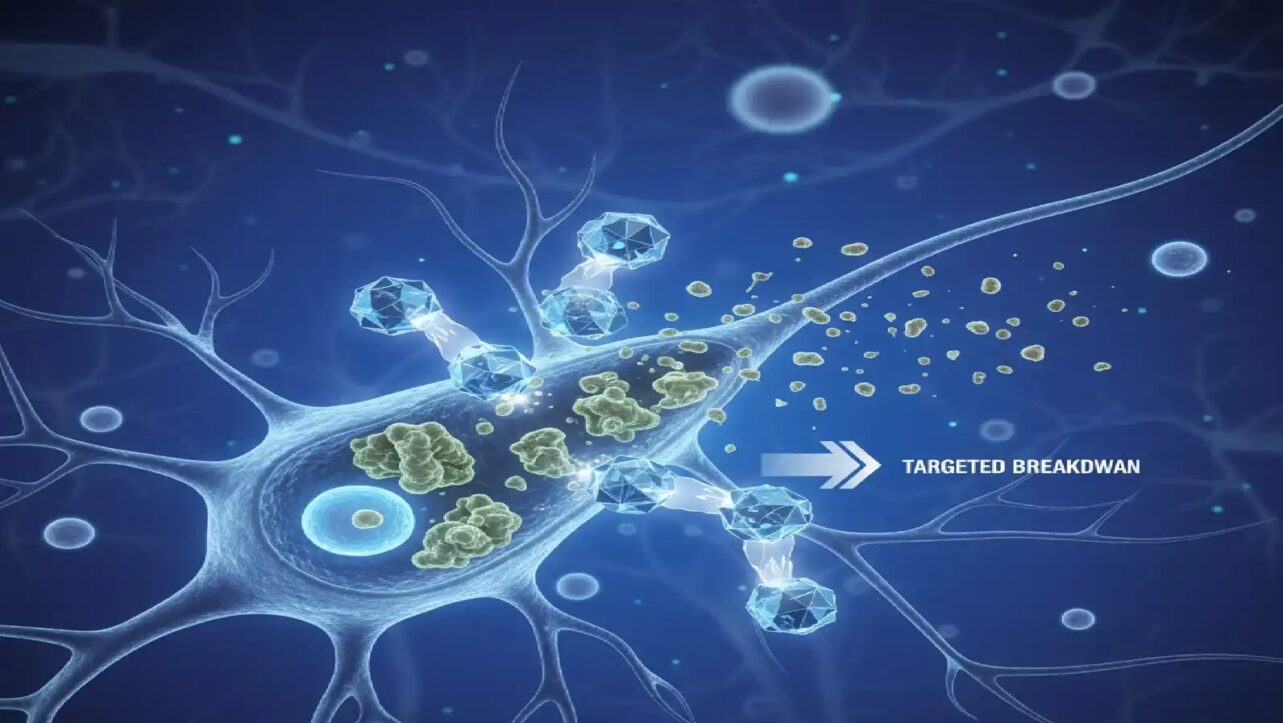
How Testicular Cancer Spreads—And Why Maddinson’s Case Is a Warning
Testicular cancer follows a predictable metastatic pathway through the lymphatic system, making its spread pattern somewhat foreseeable yet alarmingly efficient.
The first stop for metastatic disease is typically the retroperitoneal lymph nodes—the “landing zone” behind the abdomen. In Maddinson’s case, the cancer reached his abdominal lymph nodes within weeks of his initial diagnosis.
After lymph nodes, the lungs are the second most common metastatic site. Approximately one in five patients have regional lymph node spread at diagnosis, while one in eight have distant metastases, most commonly to the lungs. Other less common sites include bones, liver, and brain, with choriocarcinoma variants showing particular affinity for brain metastasis.
“It had spread to parts of my abdominal lymph nodes and lung,” Maddinson revealed. “Once I found out I had to have chemo, that was pretty hard to deal with. That was a bit where it was pretty daunting“.
The Brutal Reality of Chemotherapy
Maddinson underwent nine weeks of intensive BEP chemotherapy—a standard protocol combining bleomycin, etoposide, and cisplatin. This regimen, considered curative for metastatic testicular cancer, destroys rapidly dividing cancer cells but exacts a devastating physical toll.
“By the second or third week, I lost all my hair,” Maddinson described. “I was feeling pretty average. I was taking types of steroids to manage side effects, but they would keep me up at night. I’d sleep until about 1am, but sometimes I’d then be awake until 6am“. The crushing fatigue left him unable to perform even basic activities with his two-year-old son August.
BEP chemotherapy typically involves three to four treatment cycles, with drugs administered intravenously over several days per cycle. The number of cycles depends on cancer stage, spread extent, and response to treatment.
Despite the ordeal, BEP achieves remarkable cure rates. Over 90% of patients with good-prognosis metastatic testicular cancer are cured with three courses of BEP or four courses of etoposide and cisplatin alone.
Survival Rates: Why Time Is Everything
Testicular cancer boasts one of the highest cure rates of any malignancy when caught early, but timing dramatically impacts prognosis.
Localized disease (confined to the testicle): 99% five-year survival rate
Regional spread (lymph nodes and nearby tissues): 96% five-year survival rate
Good prognosis metastatic: More than 90% cure rate
Intermediate risk metastatic: 70-80% survival
Poor prognosis metastatic: 50-70% survival
The difference between localized and regional disease is often measured in weeks, not months—precisely why Maddinson’s case is so instructive. Even with prompt medical attention, his cancer progressed from localized to metastatic within the seven-week window between surgery and follow-up scans.
How to Perform a Testicular Self-Examination
Monthly testicular self-examinations enable early detection of abnormalities. Medical experts recommend the following technique:
Timing: Perform the exam during or immediately after a hot shower or bath, when the scrotal skin is relaxed.
Technique:
- Stand in front of a mirror to visually inspect for swelling or asymmetry
- Cup the scrotum in your palm to assess weight
- Examine one testicle at a time by gently gripping the top of the scrotum with thumb on top and fingers underneath
- Roll each testicle between thumbs and fingers of both hands, feeling for lumps or irregularities
- Check the epididymis at the back-top of each testicle—this tube structure is normal and may feel tender
What’s normal:
- Each testicle feels like a smooth, firm egg
- One testicle may be slightly larger or hang lower than the other
- No pain or discomfort during gentle handling
What’s abnormal:
- Any lump, swelling, or hardness
- Change in size, shape, or consistency
- Pain, heaviness, or aching sensation
Lumps may be as small as a grain of rice or pea initially but can grow rapidly.
The “She’ll Be Right” Attitude That Kills
Maddinson specifically addressed cultural attitudes that delay medical care, particularly among men from rural areas. “I just think it’s so important if you have anything you’re worried about, get it checked out,” he emphasized. “I grew up in the country and a lot of people fob it off. It’s a ‘she’ll be right’ attitude. Get it checked—it can make all the difference“.
This dismissive approach to symptoms—common among young men worldwide—can be lethal with testicular cancer. The aggressive nature of the disease means delays of even weeks can allow metastatic spread.
“If one person reads my story and gets checked, I’ll be happy,” Maddinson stated.
From Diagnosis to Recovery: Maddinson’s Timeline
Maddinson’s journey illustrates both the aggressive nature of testicular cancer and the effectiveness of modern treatment:
April 2025: Discovery of lump, immediate diagnosis, surgical removal
Seven weeks post-surgery: Scans reveal metastatic spread to lymph nodes and lung
Mid-May to mid-July 2025: Nine weeks of BEP chemotherapy
Late July 2025: First training session, two weeks post-chemotherapy
September 2025: Declared cancer-free
October 2025: Resuming center-wicket training with NSW squad
This compressed timeline—from diagnosis to cancer-free status in approximately five months—demonstrates both the urgency required in treatment and the remarkable curability of testicular cancer when aggressively managed.
A Message That Could Save Lives
Maddinson’s public disclosure serves a purpose beyond personal catharsis. By revealing that even immediate medical attention couldn’t prevent metastatic spread, he’s delivered a wake-up call to millions of young men who might otherwise delay seeking care.
Testicular cancer is highly treatable and often curable, even at advanced stages. But the difference between a 99% cure rate and a 70% survival rate can be measured in the days or weeks men spend convincing themselves that lump is “probably nothing”.
“To know that I caught it probably as early as I could have, and it still spread into other parts of my body, that was scary,” Maddinson said. His message is clear: don’t wait for symptoms to worsen, don’t assume youth equals invincibility, and never adopt a ‘she’ll be right’ attitude with your health.
Every man aged 15 to 35 should perform monthly testicular self-examinations and seek immediate medical evaluation for any abnormality. In the race against testicular cancer, time is the most critical variable—and unlike Maddinson, not everyone will win that race even with early detection.