An advanced artificial intelligence tool can detect tiny brain lesions causing severe epilepsy in children with up to 94% accuracy, offering faster diagnosis and potentially life-changing surgical treatment for thousands of young patients previously told their scans were normal.
The breakthrough “AI epilepsy detective,” developed by researchers at Murdoch Children’s Research Institute (MCRI) and The Royal Children’s Hospital (RCH) in Melbourne, Australia, can identify focal cortical dysplasias—brain malformations as small as a blueberry—that are routinely invisible on standard MRI scans.
80% of Diagnoses Previously Missed
Published in the journal Epilepsia, the MCRI-led study involved 71 children at RCH and 23 adults at Austin Hospital with cortical dysplasia and focal epilepsy, which causes recurring seizures. The research revealed a shocking finding: before using the AI detector, 80% of patients had their cortical dysplasia diagnosis missed by human examination of their MRI results.
“Identifying the cause early lets us tailor treatment options and helps neurosurgeons plan and navigate surgery,” said Dr. Emma Macdonald-Laurs, a RCH neurologist who led the team that created the detector.
Remarkable Success Rate Leads to Seizure Freedom
MRI and FDG-positron emission tomography (FDG-PET) scans were used to train the detector, with children separated into training and test cohorts. Using information from both MRI and PET scans, the best result was recorded in the test cohort with a success rate of 94%.
Of the 17 children in the test group, 12 underwent surgery and 11 are now completely seizure-free—a 92% surgical success rate. This represents a transformative outcome for children who previously faced a lifetime of uncontrolled seizures and progressive developmental impairment.
Why Early Detection Matters
“With more accurate imaging, neurosurgeons can develop a safer surgical roadmap to avoid important blood vessels and brain regions that control speech, thinking and movement and removing healthy brain tissue,” Dr. Macdonald-Laurs explained. “Children also avoid the need to have to undergo invasive testing“.
About one in 200 children has epilepsy, with more than 21,000 children in Victoria alone living with uncontrolled seizures. Cortical dysplasias, which develop when the baby is still in the womb, are a common cause of drug-resistant seizures affecting approximately one-third of childhood epilepsy cases.
Understanding the Hidden Threat
“The seizures usually start out of the blue during the preschool or early school years before escalating to multiple times a day,” Dr. Macdonald-Laurs said. “Children often need to attend the emergency department or be admitted to hospital for treatment. Over time, frequent seizures impact on a child’s behaviour, mood and ability to learn“.
Epilepsy due to cortical dysplasia can be improved or cured with epilepsy surgery if the abnormal brain tissue can be located and removed. However, cortical dysplasias are notoriously hard to spot on routine MRIs, with less than half being recognized on a child’s first scan.
“Cortical dysplasias can be impossible for traditional MRI techniques to identify,” Dr. Macdonald-Laurs noted. “Failure to locate the abnormal tissue slows the pathway to a definitive diagnosis and may stop a child being referred for potentially curative epilepsy surgery“.
The consequences of delayed diagnosis are severe. “The longer a child continues to have uncontrolled seizures, the more likely they are to develop learning difficulties, including intellectual disability,” she warned.
Royal’s Story: From 19 Seizures in Two Hours to Seizure-Free
Royal, now 6 years old, successfully underwent surgery after scans aided by the AI detector identified a cortical dysplasia that had been previously invisible. His mother Gurjinder described how his condition dramatically deteriorated, with seizures escalating from a couple per day to one every half hour, with the worst episode involving 19 seizures within just two hours.
“The whole ordeal took a huge toll on our family and we were struggling mentally,” Gurjinder said. Royal went from having multiple seizures a day to now being completely seizure-free following the procedure.
“Without the assistance of the detector, it would have taken so much longer to achieve a diagnosis and Royal’s health would have continued to deteriorate,” his mother stated.
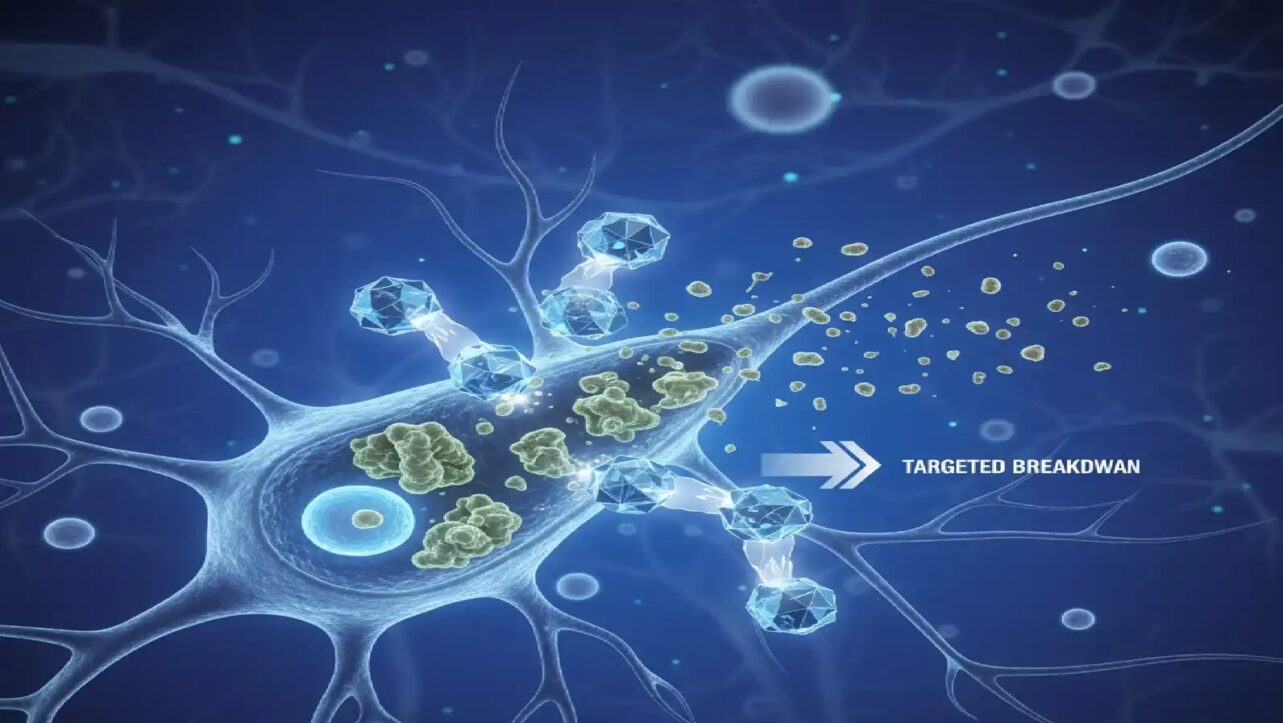
How the AI Technology Works
The AI tool was adapted from existing machine-learning frameworks developed by the Multi-centre Epilepsy Lesion Detection group, specifically tailored for bottom-of-sulcus dysplasia (BOSD) characteristics and incorporating FDG-PET data for greater precision.
Dr. Sila Genc from the MCRI Developmental Imaging Group explained that layers of advanced imaging were crucial. The combined MRI and PET scan data allowed the AI tool to detect lesions with “higher certainty” while helping surgeons avoid critical brain areas. Similar advancements in AI-powered medical imaging analysis are transforming how doctors interpret complex scans across multiple specialties.
“The tool doesn’t replace radiologists or epilepsy doctors, but it’s like a detective that helps us put the puzzle pieces together quicker so we can offer potentially life-changing surgery,” Dr. Macdonald-Laurs emphasized.
PET scans can measure brain activity and highlight regions with abnormalities in specific colors, providing complementary information to structural MRI imaging.
Flipping MRI-Negative to MRI-Positive
The researchers noted that the information provided by their MRI+PET BOSD detector can flip an “MRI-negative” patient into becoming “MRI-positive,” which has significant clinical implications including identifying surgical candidates, avoiding or improving planning of intracranial EEG monitoring, and enabling targeted surgical resection or ablation.
“At our center, increasing use of the postprocessing methods and the MRI+PET BOSD detector have increased the rate of BOSD diagnosis and decreased duration from presentation to diagnosis,” the researchers wrote in their study.
Approximately 85% of patients with BOSD who undergo complete surgical removal can be cured of epilepsy, making early and accurate detection critical.
Next Steps and Future Plans
Dr. Macdonald-Laurs said with additional funding, the team could test the detector in pediatric hospitals across Australia.
“Our next plans are to test this detector in more real-life hospital settings on new, undiagnosed patients across Australia, and also to research what children, parents, and doctors think about us using AI in their epilepsy diagnosis,” she said.
The only risk involved with the technology is the small amount of radiation children might be exposed to with PET scans, but researchers noted it was typical for PET scans to already be used in epilepsy diagnosis.
Konrad Wagstyl, a biomedical computing expert at King’s College London, called the work “really exciting” as a proof of concept and described the results as “really impressive”. His team published similar research in February 2025 using AI on MRI data that spotted 64% of epilepsy-linked brain lesions missed by radiologists.
International Collaboration
Researchers from The Royal Children’s Hospital, the University of Melbourne, Florey Institute of Neuroscience and Mental Health, Harvard Medical School, and Austin Hospital contributed to the groundbreaking study.
The full research paper, titled ‘Automated detection of bottom-of-sulcus dysplasia on MRI-PET in patients with drug-resistant focal epilepsy,‘ was authored by Emma Macdonald-Laurs, Aaron E.L. Warren, Remika Mito, Sila Genc, Bonnie Alexander, Sarah Barton, Joseph Yuan-Mou Yang, Peter Francis, Heath R. Pardoe, Graeme Jackson, and A. Simon Harvey, and published in Epilepsia with DOI: 10.1111/epi.18628.
This advancement represents a major step forward in pediatric epilepsy care, offering hope for thousands of children with previously undetectable brain lesions causing severe, drug-resistant seizures to access curative surgical treatment.