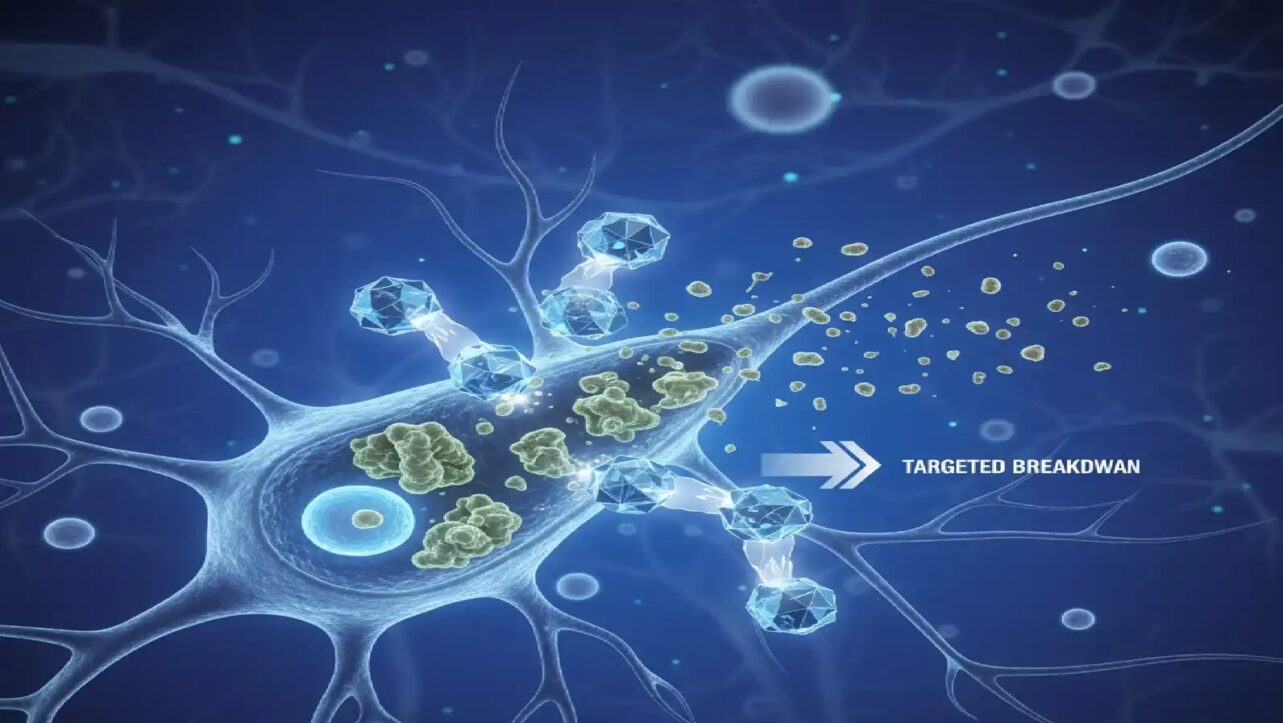
Scientists at City of Hope Research Centre have identified SMOC1 gene that drives the conversion of insulin-producing beta cells into glucagon-producing alpha cells, unveiling a critical mechanism behind type 2 diabetes progression and opening pathways for revolutionary new therapies.
Revolutionary Gene Discovery Explains Beta Cell Identity Crisis
Researchers at City of Hope, one of the largest cancer research and diabetes treatment organizations in the United States, used advanced RNA sequencing techniques to analyze pancreatic islet cells from 26 individuals—13 with type 2 diabetes and 13 without—to uncover why insulin-producing cells lose their function. The findings, published in the prestigious journal Nature Communications, reveal that SMOC1 plays a central role in beta cell dedifferentiation, a process where mature cells lose their specialized identity and transform into different cell types.
Pancreatic islets are clusters of cells that produce and release hormones into the bloodstream. Beta cells make insulin that lowers blood sugar and alpha cells make glucagon that increases blood sugar. Preserving this hormonal balance is critical for regulating normal blood sugar levels. In type 2 diabetes, some beta cells malfunction, forget their assigned job, and lose their unique traits. They start behaving more like alpha cells, making glucagon instead of insulin, causing dysregulation of blood sugar levels.
Understanding Beta Cell Transformation and AB Cells
The research team identified five distinct types of islet cells, each with unique genetic signatures and developmental trajectories. “In healthy people, islet cells can mature in different directions – some become more like alpha cells, others like beta cells,” said lead author Adolfo Garcia-Ocaña, Ph.D. “But in type 2 diabetes, the path only goes one way: beta cells start imitating alpha cells. This shift may explain why insulin levels drop and glucagon levels rise in people with the disease.“
In healthy islets, some cells follow branching pathways that could lead to maturity as either alpha cells or beta cells, suggesting flexibility in cell identity. In diabetic islets, however, this fluidity was lost; beta cells converted only into alpha cells.
Scientists also discovered unusual “AB cells” that produce both insulin and glucagon. This unusual discovery suggests these cells are able to evolve into either alpha or beta cells.
SMOC1’s Harmful Role in Beta Cells
Of the 10 genes that showed consistent activity in cells transforming from beta to alpha identity, SMOC1 stood out as a central player. However, the protein it produces did not stay where it was supposed to.
“Normally, SMOC1 is active in healthy people’s alpha cells,” explained co-corresponding author Geming Lu, MD, Assistant Research Professor. “But we saw it start showing up in the diabetic beta cells, too. It should not have been there.”
SMOC1 activity in the wrong place led to undesirable consequences: insulin production dropped, the activity of genes shaping beta cell identity slowed to a standstill and beta cells displayed markers typical of immature or alpha cells. Taken collectively, these outcomes imply that SMOC1 expression in the beta cells reduces circulating insulin, leading to higher blood sugar levels, and offer scientists a better understanding of how type 2 diabetes progresses.
“Our results indicate that SMOC1 drives beta cell dysfunction and the cells’ shift toward an alpha cell-like state,” said Dr. Garcia-Ocaña. “This helps explain why insulin levels fall and glucagon levels rise in people with type 2 diabetes.”
“The SMOC1 gene has barely been studied in diabetes,” explained Randy Kang, senior research associate. “The protein it encodes binds to growth factors that stimulate the development of tissues throughout the body. It also binds to calcium, which is required for insulin release. Based on these properties, we suspect SMOC1 strongly influences the differentiation and function of beta cells.“
Global Diabetes Epidemic Demands New Solutions
This discovery arrives as type 2 diabetes reaches epidemic proportions globally. According to the International Diabetes Federation’s 11th Edition Diabetes Atlas released in 2025, approximately 588.7 million adults worldwide are living with diabetes in 2024, a number projected to increase by 45% to 852.5 million by 2050.
In India, an estimated 89.8 million adults are currently living with diabetes as of 2024, representing a prevalence of 10.5% among the adult population. The country holds the second-highest burden of diabetes globally, with the South-East Asia region expected to experience a 73% increase in diabetes cases by 2050, rising from 106.9 million to 184.5 million. S
In the United States, approximately 38.4 million people—11.6% of the total population—have diabetes, with 38.1 million adults aged 18 years or older representing 14.7% of all U.S. adults. The North America and Caribbean region is projected to see a 21% increase in diabetes cases by 2050, rising from 56.2 million to 68.1 million. Approximately 90-95% of all diabetes cases are type 2 diabetes, and the condition disproportionately affects older adults, with prevalence reaching 29.2% among adults aged 65 and older
Clinical Implications and Future Therapeutic Strategies
The City of Hope findings suggest multiple transformative approaches for type 2 diabetes management. By mapping islet cell changes, scientists can explore ways to reverse or prevent harmful transitions before they upset blood sugar control. SMOC1 could serve as a diagnostic biomarker for beta-cell malfunction in type 2 diabetes.
Blocking SMOC1 or reversing its effects may offer new strategies to protect healthy beta-cell function and enhance insulin production in people with diabetes. Recognizing that some cells can switch types opens the door to cell-reprogramming therapies that could restore insulin production. Understanding the flexibility of AB cells and their trajectory dynamics could open avenues for new regenerative therapies.
Research Background and Next Steps
The study received funding from the Arthur Riggs Diabetes and Metabolism Research Institute at City of Hope and the George and Irina Schaeffer Gift. The laboratory of Debbie Thurmond, Ph.D., collaborated on the research with Dr. Garcia-Ocaña’s team.
In future studies, the researchers will explore how SMOC1 expression occurs in beta cells in type 2 diabetes, what regulates it, how they can control its expression, and potential agents that block SMOC1 activity. This groundbreaking discovery represents a paradigm shift from merely managing diabetes symptoms to potentially addressing the root cellular mechanisms driving disease progression.