Scientists have identified a missing molecule in Down syndrome brains that could potentially be restored to improve cognitive function even in adulthood—a breakthrough that challenges decades of assumptions about the irreversibility of the condition’s neurological effects.
The Discovery
Researchers from the Salk Institute for Biological Studies and the University of Virginia School of Medicine found that faulty brain circuits in Down syndrome may stem from a deficiency of pleiotrophin, a protein essential for nervous system development and function. The groundbreaking study, published in the journal Cell Reports, demonstrates that restoring this molecule improved brain function in adult mice long after their brains had fully formed.
“This study is really exciting because it serves as proof-of-concept that we can target astrocytes, a cell type in the brain specialized for secreting synapse-modulating molecules, to rewire the brain circuitry at adult ages,” said Dr. Ashley N. Brandebura, who conducted the research at Salk Institute and now continues her work at UVA Health’s Brain Institute.
Why This Matters
Down syndrome, caused by trisomy 21, affects approximately 1 in 640 live births in the United States and results in developmental delays, cognitive impairments, and various physiological challenges. Previous attempts to enhance brain circuits in Down syndrome required intervention at extremely precise and brief windows during pregnancy, making them impractical and risky.
The new approach offers a significant advantage: it works in adults, potentially eliminating the need for prenatal intervention altogether. This opens possibilities for treating existing patients rather than requiring treatment during the narrow developmental window in the womb.
The Science Behind It
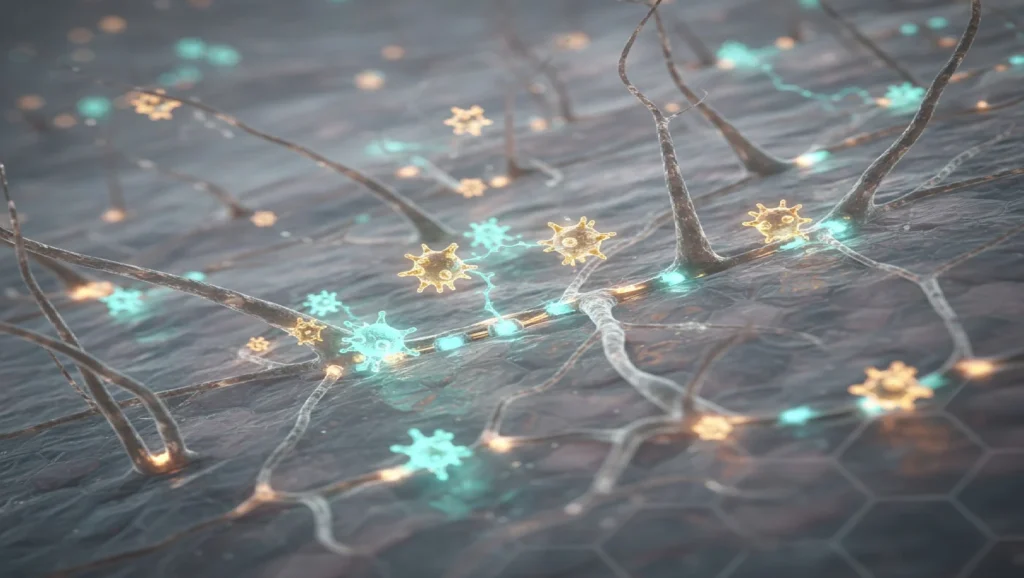
The research team used a Down syndrome mouse model (Ts65Dn line) to map protein expression patterns in the brain. They discovered that pleiotrophin levels were markedly diminished in Down syndrome brains, particularly in astrocytes—specialized glial cells that maintain the chemical environment around neurons and secrete molecules crucial for synapse formation.
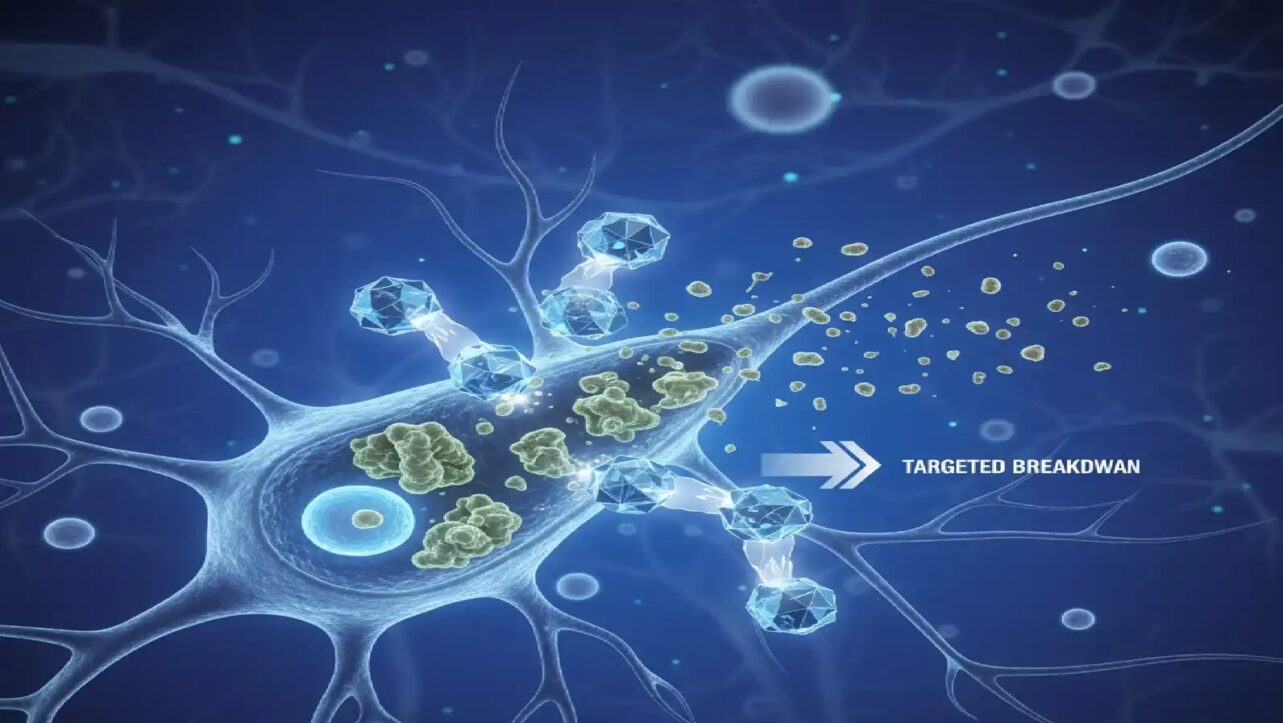
To test their hypothesis, the scientists employed viral vectors—engineered viruses stripped of harmful components—to deliver the gene encoding pleiotrophin specifically to astrocytes in the hippocampus, the brain region vital for memory and learning. This targeted approach allowed precise delivery without systemic side effects.
Remarkable Results
The results were striking: pleiotrophin delivery led to pronounced increases in synapse number and enhanced synaptic plasticity—the brain’s adaptive capacity underlying learning and memory. The treatment corrected dendrite structure, increased synapse density, and improved functional synaptic signaling in the hippocampus.
“This is still far off from use in humans, but it gives us hope that secreted molecules can be delivered with effective gene therapies or potentially protein infusions to improve quality of life in Down syndrome,” Brandebura explained.
Targeting Astrocytes: A Paradigm Shift
For decades, astrocytes were considered mere “support staff” for neurons, but recent research has revealed they are active regulatory players that modulate neural network function and influence brain plasticity. The study’s lead researcher, neuroscientist Dr. Nicole J. Allen from the Salk Institute, has been systematically investigating how proteins secreted by astrocytes at different life stages modulate synapse stability and renewability.
By focusing on astrocytes as therapeutic targets, the team discovered a novel mechanism to promote brain plasticity that leverages these cells’ natural secretory capacities to influence synaptic connections dynamically.
Beyond Down Syndrome
While pleiotrophin deficiency is unlikely to be the sole cause of brain circuit problems in Down syndrome, the implications extend far beyond this condition. The astrocyte-mediated delivery strategy could benefit other disorders characterized by synaptic dysfunction, including fragile X syndrome, and potentially neurodegenerative conditions like Alzheimer’s disease, which involves progressive synaptic loss.
Funding and Next Steps
The research received support from the Chan Zuckerberg Initiative and the National Institutes of Health’s National Institute of Neurological Disorders and Stroke. While the approach remains far from clinical use in humans, it represents a crucial proof-of-concept that adult brain circuits can be rewired through targeted molecular interventions.
The findings challenge long-held assumptions about the fixed nature of brain architecture after early development and suggest that adult interventions may prove both viable and impactful for treating cognitive impairments associated with genetic disorders.