When 25 people were hospitalized with life-threatening botulism in North East England between May and June 2025, it wasn’t just another medical incident—it was a warning signal about a global crisis hiding in plain sight.
The outbreak, detailed in a groundbreaking Eurosurveillance study published October 2nd, 2025, exposed catastrophic failures in an industry projected to reach $190.5 billion by 2030—yet remains largely unregulated across most of the world.
A Global Pattern of Preventable Deaths
The English outbreak is far from isolated. Over just seven weeks in mid-2025, more than 40 cases of botulism linked to cosmetic Botox injections were reported across the U.S. and UK—including at least 12 cases in Massachusetts, one in Oregon, and 28 in England. Meanwhile, a Kentucky medical spa admitted using illegally imported Botox from Korea and Turkey for four years, leaving customers to spend nearly $25,000 treating side effects from contaminated injections.
Since 2019, UK regulators have recorded a fourfold increase in suspected Botox complications—from 52 cases in 2019 to 225 in 2024, with 141 cases already reported by September 2025. During this period, 12 deaths have been linked to botulinum toxin treatments.
These aren’t anomalies. They’re symptoms of an industry where profit has outpaced patient safety on a massive scale.
The $190 Billion Regulatory Black Hole
The global non-invasive aesthetic treatment market was valued at $61.2 billion in 2022 and is projected to explode to $190.5 billion by 2030, growing at an annual rate of 15.4%. Injectable procedures—including Botox and dermal fillers—account for more than 63% of this market.
According to the ISAPS 2024 Global Survey, Botox use surged by 845% between 2000 and 2018 in the United States alone, with nearly 19 million non-surgical aesthetic procedures performed globally each year. Yet this rapid expansion has occurred with minimal regulatory oversight in most jurisdictions.
The UK aesthetics market, valued at £3 billion and growing to £3.6 billion by 2025, remains “effectively unregulated,” according to industry analysts. Anyone can legally administer Botox regardless of training or qualifications, as no license is legally required for non-surgical cosmetic procedures.
Australia’s cosmetic injectable industry, worth approximately AU$6 billion, operates under similarly fragmented regulations, with prescription validity periods varying wildly between states—six months in New South Wales versus 12 months in Victoria and Queensland.
India’s Explosive Growth Masks Deadly Safety Gaps
India recorded a staggering 1.29 million aesthetic and cosmetic procedures in 2024—a record high that places the country among the top 10 globally for such treatments. Non-surgical procedures including Botox and dermal fillers alone reached 610,000 treatments, representing a 7% increase over the previous year.
The Indian anti-ageing market has grown to $2.5 billion in 2024 and is projected to reach $4 billion by 2033, fueled by social media influence and rising consumer awareness of cosmetic procedures.
But this explosive growth has come with a devastating human cost. In July 2025, actress and model Shefali Jariwala died reportedly following anti-ageing injections. A woman in Kerala lost her fingers and toes in February 2025 after a liposuction procedure went wrong. A man died in Kanpur after a hair transplant procedure.
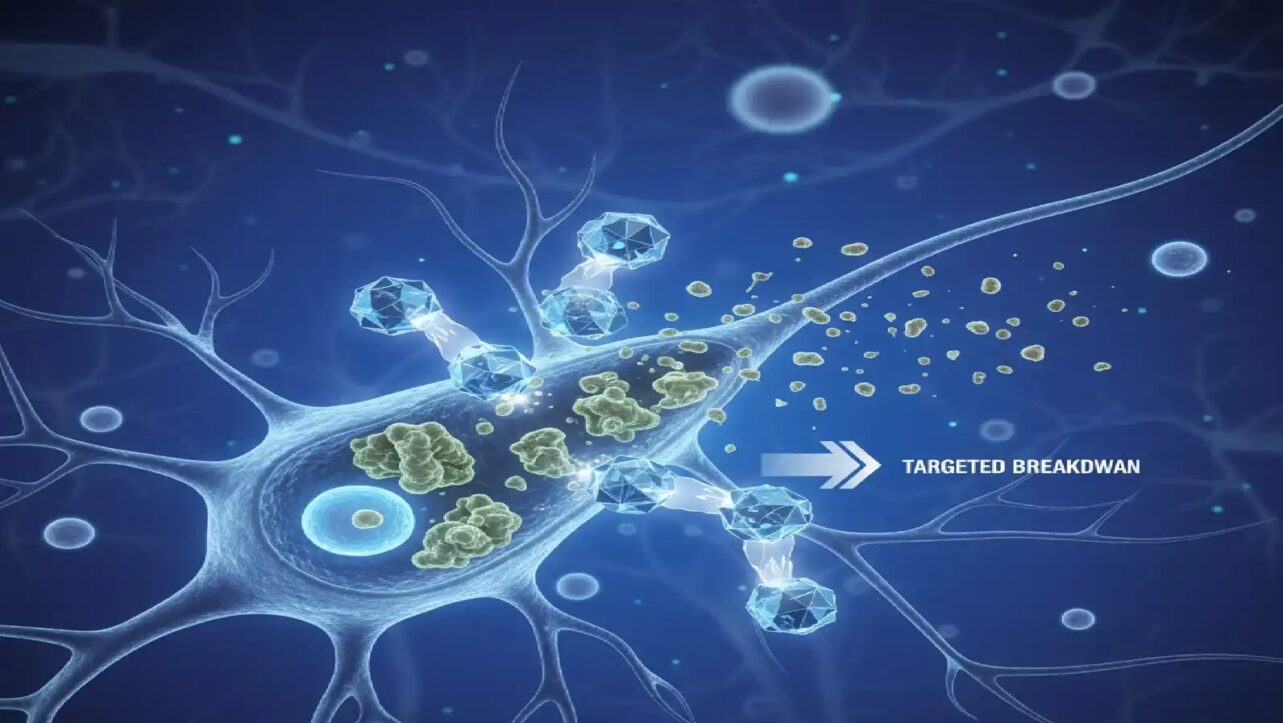
“Unlicensed and untrained personnel are administering treatments such as Botox,” said Dr. Smriti Naswa Singh, consultant in dermatology and cosmetology at Fortis Hospital, Mumbai. “Botox is a muscle-paralysing agent. If injected into the wrong muscle group, it can lead to facial asymmetry, like a drooping eyebrow or uneven smile. In the hands of untrained individuals, it can lead to serious consequences“.
In some cases documented in India, Botox administered in doses 20 to 30 times higher than recommended has caused botulism, which can lead to death. Not following aseptic precautions can result in infections, hematomas, bleeding, pain, and bruising.
The problem extends beyond untrained practitioners. In 2010, an undercover investigation by India Today exposed how easily fake Chinese Botox—claiming “Chinese FDA approval” from a non-existent regulatory body—flooded the Indian market. Dealers claimed to supply doctors across Delhi, Pune, Mumbai, and Hyderabad, and even export to America.
The England Outbreak: A Case Study in Systemic Failure
The North East England outbreak crystallized everything wrong with the current system. Researchers comparing 21 hospitalized patients with 29 individuals who received safe cosmetic injections uncovered shocking disparities:
Zero percent of botulism victims reported receiving consent forms or safety information—compared to over 80% who received legitimate treatments. Only 15% of victims reported their practitioner washing hands, versus 76% of the control group.
Many injections occurred in domestic settings—bedrooms and kitchens—eliminating any pretense of clinical oversight. The unlicensed product used, labeled as containing 200 units per vial, actually contained approximately 370 units—85% more potent than stated.
All 25 victims required hospitalization. Sixteen needed emergency botulism antitoxin treatment to prevent complete paralysis. Symptoms included blurred vision (92%), extreme fatigue (92%), difficulty swallowing (88%), and breathing difficulties.
How Illegal Products Flood the Market
Since May 2023, UK authorities have seized more than 4,700 vials of unlicensed botulinum toxin at borders and inland locations. Almost all originated from South Korea, including brands such as Botulax, reNTox, Innotox, and Toxpia—none authorized for UK sale.
A September 2025 BBC undercover investigation documented nurses exchanging prescriptions via WhatsApp, pharmacists instructing clients to falsify medical records, and a fraudulent doctor selling Korean toxin vials for cash—all without face-to-face consultations.
One London pharmacist told undercover investigators: “We can just do it as if we did the face-to-face today… I’ve just done it,” while selling Botox without any medical examination. When questioned about legality, he replied: “Yeah, you’re going to do it… That’s what you’re doing“.
In 2024, the FDA discovered counterfeit Botox circulating across multiple U.S. states, warning that fake versions posed serious health risks.
Criminal Networks and Legal Loopholes
Under UK law, anyone involved in supplying unlicensed botulinum toxin faces up to two years in prison and unlimited fines. Yet prosecutions remain rare.
Andy Morling, head of the UK MHRA’s Criminal Enforcement Unit, stated: “Anyone involved in the supply of unlicensed botulinum toxin—whether through organized networks or informal sales from kitchen tables, hair salons, or via social media—is breaking the law and endangering lives“.
By August 2025, UK authorities had confirmed 41 cases of iatrogenic botulism across five regions, with 32 requiring hospitalization and eight needing intensive care. Yet the underground market continues expanding.
What Consumers Need to Know
Health authorities urge the public to recognize warning signs of unsafe cosmetic procedures:
- Botulinum toxin offered without medical consultation
- Treatments in informal settings (homes, hair salons, mobile services)
- Prices significantly below market rates
- Practitioners unable to verify product licensing
- No consent forms or safety information provided
Botulism symptoms can take up to four weeks to develop after cosmetic procedures. Anyone experiencing difficulty swallowing, slurred speech, or breathing difficulties after receiving botulinum toxin injections should seek immediate medical attention.
The Industry’s Reckoning
The England outbreak represents a tipping point. As the cosmetic injectables industry races toward $190 billion, the gap between market growth and regulatory oversight has become a public health emergency spanning continents.
From the UK’s botulism clusters to India’s record 1.29 million procedures amid rising deaths from unregulated treatments, the pattern is clear: explosive market expansion without corresponding safety infrastructure creates preventable tragedies.
Dr. Gauri Godbole, Consultant Medical Microbiologist at UK Health Security Agency, emphasized: “These cases highlight the urgent need for improved practitioner training, insurance standards, and product safety in the rapidly expanding cosmetic injectables industry“.
Until comprehensive international regulations close the loopholes that allow untrained practitioners to inject unlicensed neurotoxins in domestic settings—and until countries like India establish dedicated regulatory frameworks for aesthetic medicine—more preventable deaths will follow.
The question is no longer whether the cosmetic injectables industry needs regulation—it’s how many more lives will be lost before governments act decisively.