A 65-year-old retired speech and language therapist has made headlines worldwide after playing the clarinet during a four-hour brain surgery at London’s King’s College Hospital, demonstrating the immediate effectiveness of Deep Brain Stimulation (DBS) treatment for Parkinson’s disease.
Instant Improvement on the Operating Table
Denise Bacon from Crowborough, East Sussex, experienced immediate improvements in her finger movements as electrical impulses were delivered to her brain during the groundbreaking procedure performed by Professor Keyoumars Ashkan, a neurosurgery expert. The surgery, which took place in October 2025, allowed medical professionals to witness—and hear—the instant results of the treatment.
“I remember my right hand being able to move with much more ease once the stimulation was applied, and this in turn improved my ability to play the clarinet, and I was delighted,” Bacon shared in a hospital release.
The Surgical Procedure
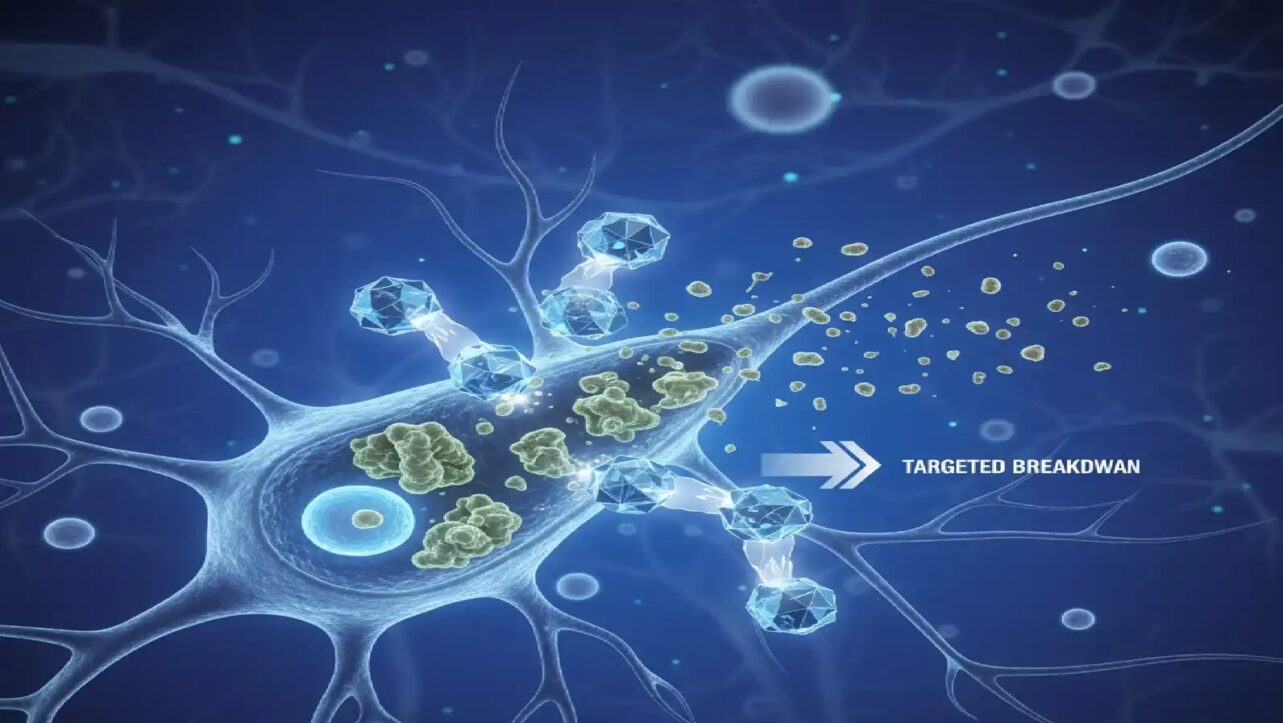
Deep Brain Stimulation involves implanting electrodes into specific deep structures of the brain to modify brain activity and reduce symptoms in patients with treatment-resistant movement disorders such as Parkinson’s disease. During the procedure, holes half the size of a five pence piece were made in Bacon’s skull after a frame with precise coordinates was placed on her head, acting as a navigational guide to the correct positions within the brain.
While the brain itself has no pain receptors, Bacon received a local anesthetic to numb her scalp and skull and remained awake throughout the entire operation so her symptoms could be monitored in real-time. The electrodes were connected to a pulse generator, similar to a pacemaker, which was implanted in her chest to deliver continuous electrical impulses.
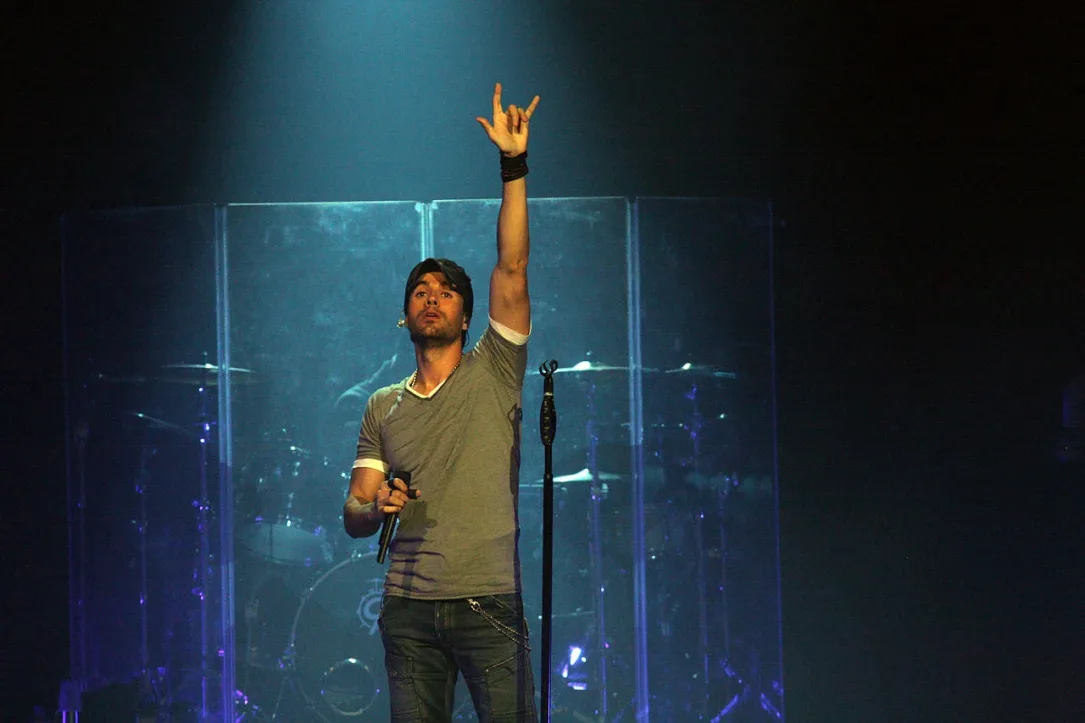
A Musical Journey Back to Life
Diagnosed with Parkinson’s disease in 2014, Bacon had experienced progressive symptoms including slowness of movement (bradykinesia) and muscle stiffness (rigidity), which severely affected her ability to walk, swim, dance, and play her beloved clarinet. She had been forced to stop playing with the East Grinstead Concert Band five years ago due to her deteriorating symptoms.
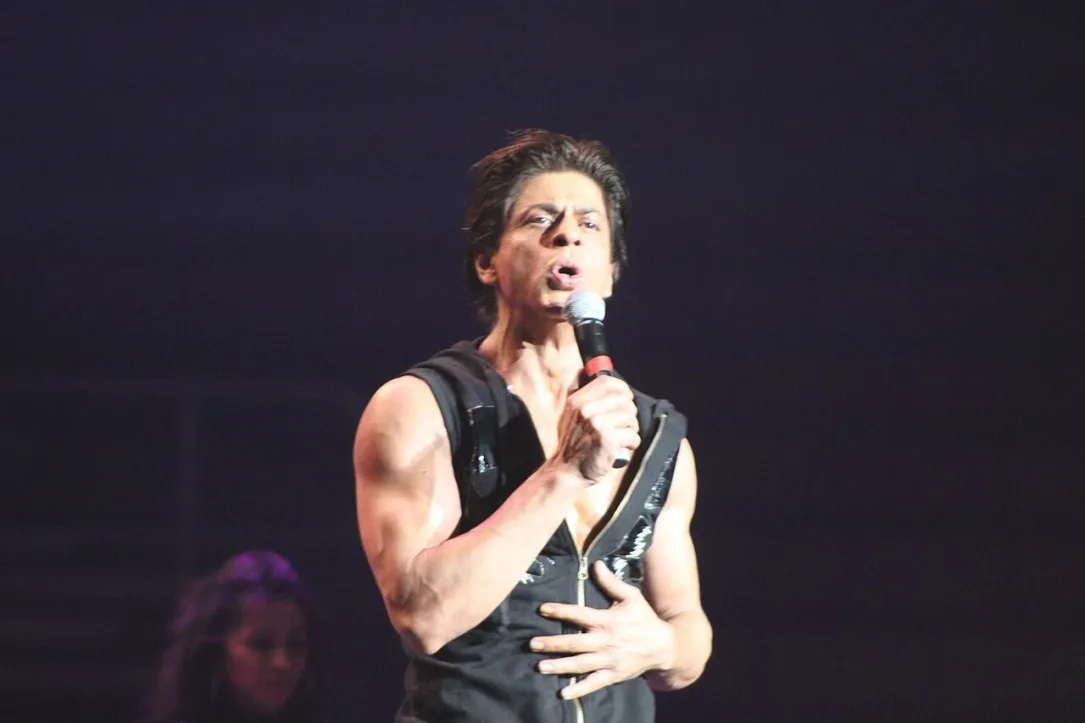
“As a keen clarinettist, it was suggested Denise bring her clarinet into the operating theatre to see whether the procedure would improve her ability to play, which was one of Denise’s main goals for the surgery,” Professor Ashkan explained. “We were delighted to see an instant improvement in her hand movements, and therefore her ability to play, once stimulation was delivered to the brain“.
Personalized Medicine Approach
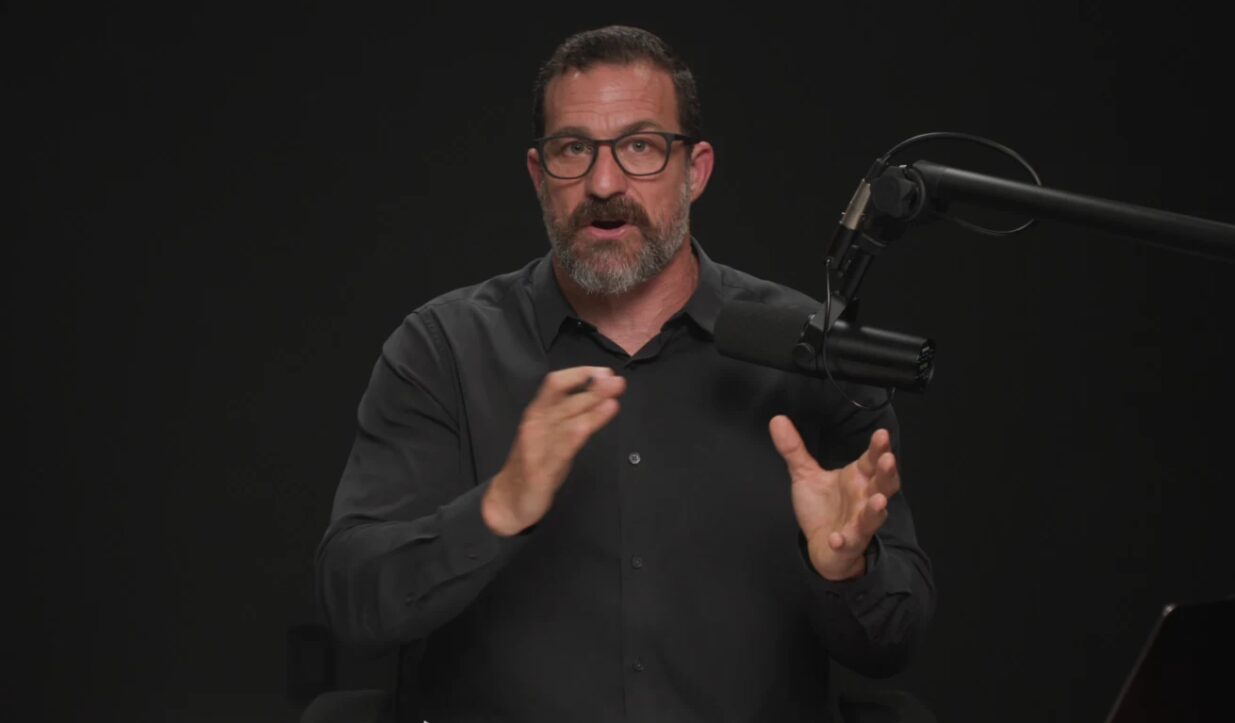
Professor Ashkan emphasized his approach to such procedures: “I try to understand the factors that will bring back quality of life that was lost because of Parkinson’s disease“. Before every surgery, he conducts a goal-setting exercise with patients to understand what specific activities matter most to their quality of life.
“This is what we call personalized medicine. For every patient there is a goal, everybody’s different, everybody has different aspects to what they consider as key to the quality of life,” Ashkan explained during a post-surgery interview. This personalized treatment approach is designed to last many decades, giving patients like Bacon renewed hope and improved quality of life.
Immediate and Long-Term Benefits
Bacon described the experience as initially making her feel “quite sceptical,” saying she didn’t think “it would be possible to play the clarinet laying on the operating table“. However, the results exceeded her expectations, with immediate improvements visible during the surgery itself.
“I can walk normally. I was walking normally straight after the surgery, and life’s just opened up again. It feels like there’s a future,” Bacon shared. She has already reported improvements in her walking ability and is eagerly anticipating returning to swimming and dancing.
According to King’s College Hospital, the chest-implanted pulse generator will continue supporting Bacon for the next two decades by continuously delivering electrical impulses. Bacon opted for the rechargeable type of pulse generator battery, which can last up to 20 years before requiring replacement. The innovative generator will monitor her brain activity and can help automatically adjust the stimulation when needed.
A Continuing Tradition
This procedure at King’s College Hospital continues a remarkable tradition of music-guided brain surgeries. In 2020, Professor Ashkan performed a similar operation where a violinist played jazz standards while a tumor was removed from her brain. The approach demonstrates how medical innovation combined with personalized patient care can restore lost abilities and dramatically improve quality of life for individuals living with Parkinson’s disease.
The successful outcome of Bacon’s surgery showcases the power of Deep Brain Stimulation as a treatment option for Parkinson’s patients who have lost cherished abilities due to their condition.