Scientists have developed a revolutionary nanobody-based antivenom that protects against bites from 17 different African snake species, marking the first product-ready recombinant snakebite treatment that outperforms century-old traditional antivenoms. The breakthrough research, published in Nature on October 20, 2025, could transform treatment for a neglected tropical disease that kills 140,000 people annually and leaves over 400,000 with permanent disabilities.
Eight Nanobodies Replace Complex Animal Sera
Researchers from the Technical University of Denmark (DTU) and Liverpool School of Tropical Medicine developed the antivenom by immunizing an alpaca and a llama with venoms from 18 different African snake species, including cobras, mambas, and rinkhals. Using advanced phage display technology, the team extracted RNA from blood samples and isolated genes that produce nanobodies—small, stable antibody fragments naturally found in camelid species.
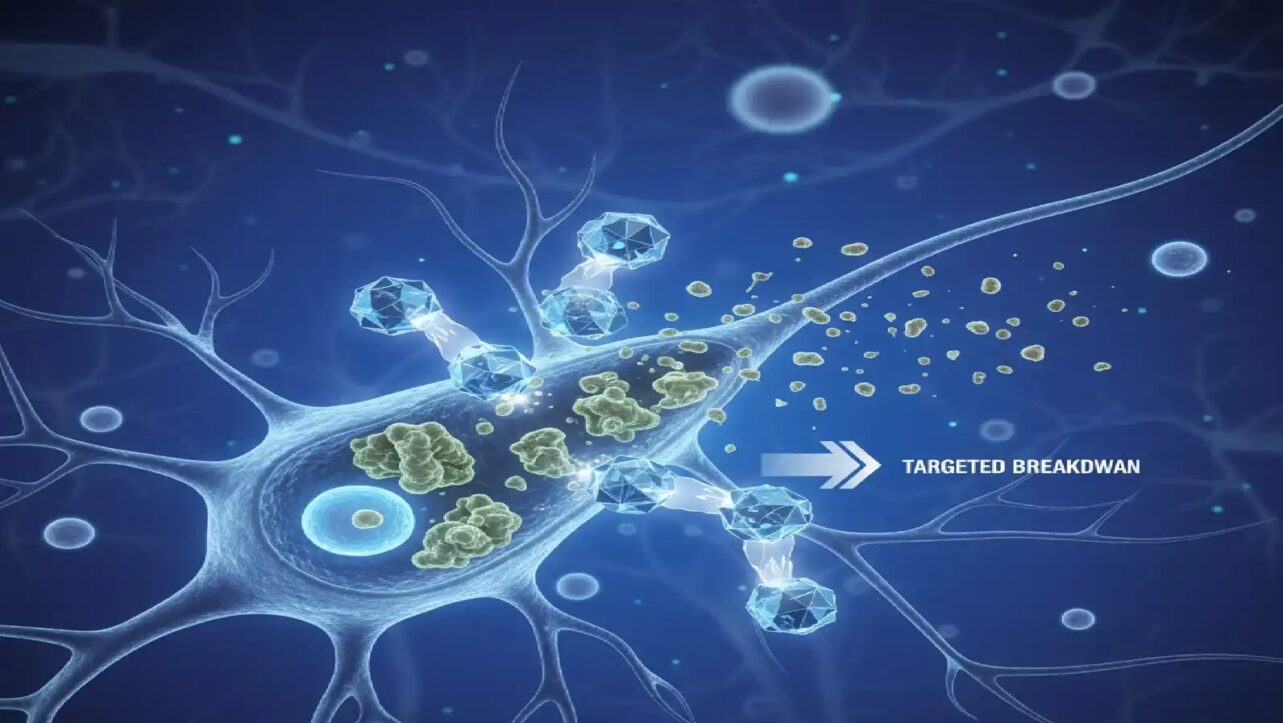
The final formulation combines just eight carefully selected nanobodies that together neutralize seven key toxin subfamilies found across African elapid snakes. This precision targeting represents a paradigm shift from traditional antivenoms, which contain large, undefined mixtures of antibodies where only a small proportion actually neutralize the most dangerous toxins.
Superior Performance in Preclinical Testing
In mouse studies, the recombinant antivenom successfully prevented death from 17 out of 18 tested snake species, with only one green mamba species partially resistant. The formulation demonstrated particular promise against the black mamba, forest cobra, Cape cobra, and spitting cobra—species whose venoms contain dramatically different toxin profiles.
The antivenom also showed superior performance against the commercial product Inoserp PAN-AFRICA in preventing both mortality and skin necrosis across all tested snake species. However, researchers noted that venoms from black mamba and forest cobra were only partially neutralized when the antivenom was administered after venom exposure, highlighting that timing remains critical.
Breakthrough in Preventing Tissue Damage
A major advantage of the nanobody approach is superior tissue penetration compared to conventional antibodies. Nanobodies penetrate tissue faster and deeper than the larger antibodies in current antivenoms, effectively reducing tissue damage even with delayed treatment. Traditional antivenoms have demonstrated only limited effectiveness against local tissue damage, which frequently leads to amputations in snakebite survivors.
Safer Treatment with Lower Side Effect Risk
The recombinant antivenom carries a much lower risk of serious immune reactions compared to traditional horse serum-derived products. Current antivenoms frequently produce adverse side effects in patients due to the introduction of large, heterogeneous antibody mixtures from animal plasma. The nanobody approach could enable clinicians to start treatment earlier without waiting for clear symptoms to avoid triggering dangerous immune reactions.
Professor Nicholas Casewell, Director of LSTM’s Centre for Snakebite Research & Interventions, emphasized: “For more than a century, antivenoms have been made using animals, and while these products save lives, they come with serious limitations. The recombinant nanobody approach enables us to target venom toxins in a precise manner, which should lead to a safer, more consistent, and scalable therapy“.
Half the Cost of Current Antivenoms
The manufacturing approach offers significant economic advantages for resource-limited regions where snakebite burden is highest. Professor Andreas Hougaard Laustsen-Kiel from DTU estimates the antivenom can be produced at less than half the current price because less active substance is needed to achieve the same effect. Additionally, nanobodies possess very high physical stability, which could dramatically lower storage and distribution costs in tropical climates.
Traditional recombinant IgG-based antivenoms cost between USD 20-225 per treatment to manufacture, while conventional horse serum products range from USD 2.40 to USD 25 per 10mL vial depending on production volume. The nanobody approach’s scalability and consistent quality could make effective treatment accessible to rural communities currently underserved by existing supply chains.
Timeline to Market
While the antivenom shows exceptional promise in preclinical studies, it has not yet been tested in humans. The research team is currently upgrading nanobody components and fine-tuning the formulation to provide even better protection against species like the black mamba where partial neutralization was observed.
Professor Laustsen-Kiel stated: “We have already upgraded one of the nanobodies included and are in the process of improving another. We are constantly learning new things along the way, and it may turn out that some minor adjustments will need to be made in the future“. Clinical trials could begin in one to two years with the right support, while a finished product could potentially be ready within three to four years.
Addressing a Neglected Tropical Disease
Snakebite envenoming is classified by the World Health Organization as one of 21 neglected tropical diseases, causing between 100,000 and 150,000 deaths worldwide annually. Three times as many people survive with serious disabilities, including amputations and permanent tissue damage. The burden falls overwhelmingly on rural communities in sub-Saharan Africa and South Asia where access to effective and affordable treatment remains severely limited.
The complexity of African snake venoms has historically made comprehensive protection particularly challenging. In Central Africa, where multiple venomous species coexist, the Cape cobra’s neurotoxin-rich venom paralyzes the nervous system while the spitting cobra’s cytotoxin-rich venom causes tissue breakdown leading to amputations. This variation means antivenoms effective against one species often fail against another.
Challenging Conventional Wisdom
The research demonstrates that broad snakebite protection can be achieved with just eight nanobody components, challenging the long-held belief that mixtures of a large number of antibodies are necessary for effective treatment. Joseph Jardine, a protein engineer and immunologist at Scripps Research Institute who was not involved in the research, praised the achievement: “To find eight recombinant monoclonals that all work together to neutralize the critical toxins, that was a huge achievement”.
The modular platform validated by this research shows that defined antibody mixtures can replace complex animal products, opening pathways for safer, more effective, and more equitable snakebite treatment globally. Future research will focus on improving the antivenom’s durability and testing its safety in clinical settings before widespread deployment.