Researchers have achieved a significant breakthrough by using an advanced form of CRISPR technology to restore sight in mice born with inherited blindness, offering new hope for treating genetic eye diseases that currently have no cure. The study, published in Nature Communications in March 2025, demonstrates that “prime editing”—a newer, more precise gene editing technique—can permanently fix the DNA errors causing retinitis pigmentosa, the most common inherited cause of blindness.
While still years away from human application, the research represents a major step forward in treating genetic vision loss that affects approximately 1 in 4,000 people worldwide.
Why This Gene Editing Is Different
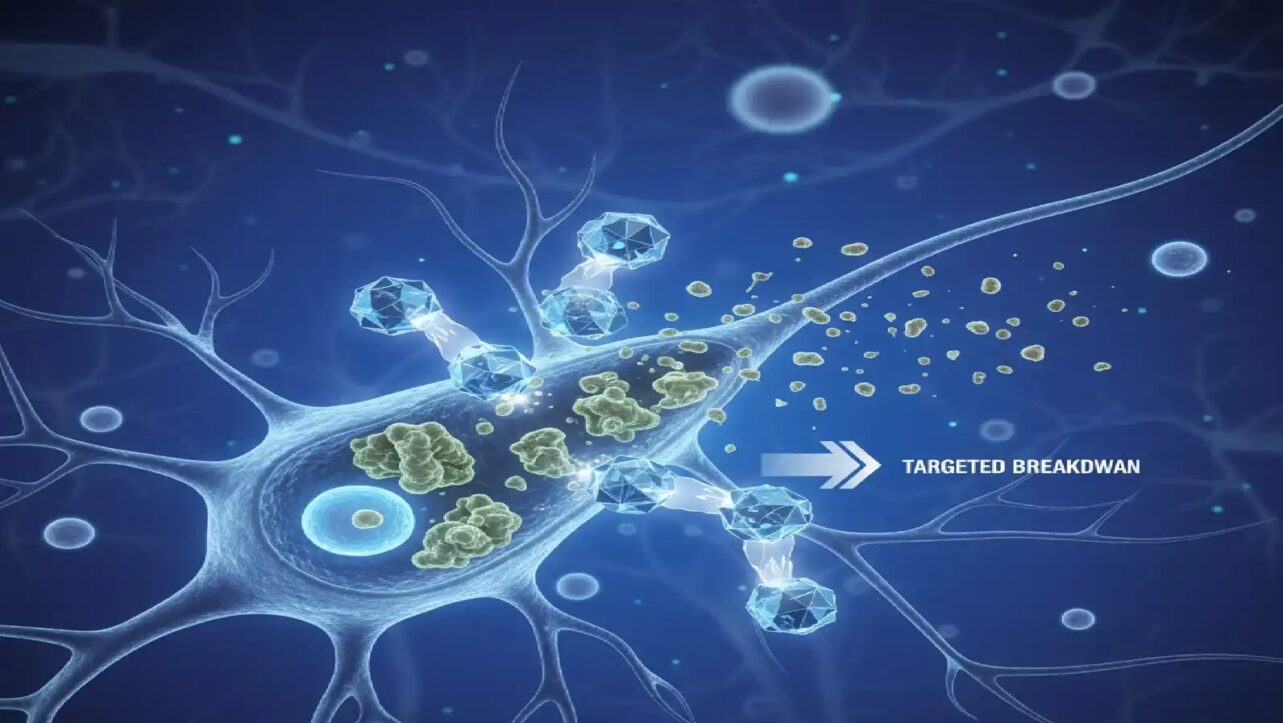
Prime editing works like a molecular word processor, rewriting mutated DNA letter by letter without completely breaking the DNA strands. This matters because earlier CRISPR techniques required cutting both strands of DNA, which could cause unintended genetic changes.
“Prime editing is adept at correcting point mutations precisely with high editing efficiency and rare off-target events,” the researchers explained. Point mutations—single-letter errors in genetic code—cause half of all genetic diseases but have historically been extremely difficult to correct.
Previous approaches to treating genetic eye diseases worked by adding a healthy copy of a gene without fixing the broken one. Prime editing actually corrects the original mistake at its source, offering a permanent solution rather than a temporary workaround.
The Results in Mice
The research team treated one-week-old mice carrying a genetic mutation that causes retinitis pigmentosa by delivering the prime editing system directly into their eyes. The outcomes were striking:
Vision was restored in treated mice—they could distinguish light from dark, avoided visual cliffs in behavioral tests, and showed pupil constriction responses that were nearly absent in untreated blind mice.
Photoreceptor cells survived instead of dying. Treated mice maintained four healthy layers of light-sensing rod cells compared to just one incomplete layer in blind mice. Rod cells are responsible for night vision and peripheral vision.
Only 26% correction was needed to achieve these results. Even though just over a quarter of cells had their DNA successfully corrected, this was enough to restore 39% of normal protein levels and significant vision function. This surprising efficiency means only a fraction of cells need fixing to restore meaningful sight.
Improvements lasted at least eight weeks after a single treatment, with protective effects persisting long-term.
The Target: Retinitis Pigmentosa
Retinitis pigmentosa (RP) affects approximately 1 in 4,000 people globally, making it the leading cause of inherited vision loss. The disease typically begins with night blindness during adolescence, progresses to tunnel vision in young adulthood, and can eventually lead to complete blindness.
Currently, no effective treatment exists for the vast majority of RP patients. While one FDA-approved gene therapy is available, it only works for patients with mutations in a specific gene called RPE65—representing just 2% of RP cases.
The genetic complexity of RP presents a major challenge: over 100 different genes can cause the disease when mutated. The mutation corrected in this study affects the PDE6B gene, one of several major causes of the condition.
Why Eyes Are Ideal for Gene Editing
The eye represents an ideal testing ground for gene editing therapies for several reasons :
Direct delivery – Doctors can inject treatments straight into the eye without affecting the rest of the body, avoiding systemic side effects. The researchers confirmed no leakage of the gene editing system into other organs.
Immune protection – The eye has special immune privileges that make it less likely to reject foreign genetic material.
Easy monitoring – Vision improvements can be measured objectively through standard eye tests, unlike many other genetic conditions.
Small doses – The enclosed space of the eye requires much smaller amounts of medicine than treating diseases affecting the entire body.
Safety Profile Looks Strong
One of the biggest concerns with any gene editing technology is “off-target effects”—unintended changes to DNA in the wrong places. The researchers used two sophisticated detection methods to search for these mistakes and found essentially none.
“Treatment with the PE system in vivo greatly restores protein expression and protects rod cells from degeneration with negligible off-target effects,” the study authors reported.
The prime editing system showed high specificity, making changes only at the intended target site while leaving the rest of the genome untouched.
Related Human Trials Show Promise
While this specific prime editing approach is still in animal testing, related CRISPR eye therapies are already being tested in humans with encouraging early results.
A clinical trial testing standard CRISPR gene editing for Leber congenital amaurosis—another inherited cause of blindness—reported positive outcomes in late 2024. In that study, 11 of 14 participants experienced measurable vision improvements on at least one test, with six people improving on multiple vision measures.
“This research demonstrates that CRISPR gene therapy for inherited vision loss is worth continued pursuit in research and clinical trials,” concluded Harvard Medical School researchers leading that trial. The safety profile from those human trials has been reassuring, with CRISPR-based therapy delivered directly into the eye proving both safe and effective.
What Needs to Happen Before Human Testing
Several important steps remain before this prime editing approach can be tested in people :
Improved delivery system – The current method requires two separate virus particles to deliver all the components. Researchers aim to package everything into a single delivery vehicle for greater efficiency.
Better targeting – Using eye-specific genetic switches could ensure the editing machinery only activates in the right cell types.
Additional safety testing – Extensive evaluation in more animal models must precede human studies.
The researchers noted that recent improvements in prime editing technology have enhanced both safety and efficiency, with newer systems showing “great performances” in laboratory tests.
Beyond One Disease
This breakthrough validates prime editing as a viable approach for correcting genetic diseases, not just in the eye but potentially throughout the body. The eye serves as a proving ground for techniques that could eventually treat genetic conditions affecting other organs.
Beyond retinitis pigmentosa, prime editing could potentially treat other inherited eye diseases including Leber congenital amaurosis, Stargardt disease, and various retinal dystrophies.
“This study provides a therapeutic opportunity for the use of prime editing to correct mutated genes at the genomic level,” the researchers concluded. “Extensive preclinical investigations in ocular gene-based interventions have demonstrated significant therapeutic potential, with multiple successful transitions from experimental models to clinical-stage human studies“.
For the millions living with inherited retinal diseases, these advances represent important progress toward treatments that could one day prevent or reverse genetic blindness through one-time gene correction therapies.
Key Takeaways:
- Prime editing corrected DNA mutations causing inherited blindness in mice without harmful side effects
- Treated mice regained significant vision with just 26% of retinal cells corrected
- Retinitis pigmentosa affects 1 in 4,000 people with no current effective treatment for most patients
- Similar CRISPR eye therapies already showing promise in early human trials
- Multiple steps remain before this specific approach reaches human testing