A groundbreaking advancement in vision restoration has emerged from Stanford Medicine, marking a pivotal moment for millions suffering from advanced age-related macular degeneration (AMD). Researchers have successfully developed and clinically tested a tiny wireless retinal implant, named PRIMA, which, when paired with advanced smart glasses, partially restores functional vision in patients who previously faced incurable blindness.
The PRIMA system represents the first effective eye prosthesis capable of restoring “form vision”—the ability to recognize shapes, patterns, and letters rather than just light perception. This remarkable achievement was demonstrated in an international clinical trial involving 38 participants over the age of 60, all affected by geographic atrophy, a severe form of AMD that gradually destroys central vision. The findings, published on October 20 in the New England Journal of Medicine, showed that 27 out of 32 patients who completed the trial regained the ability to read, with many achieving visual acuity nearing 20/42—an extraordinary recovery for this patient group.
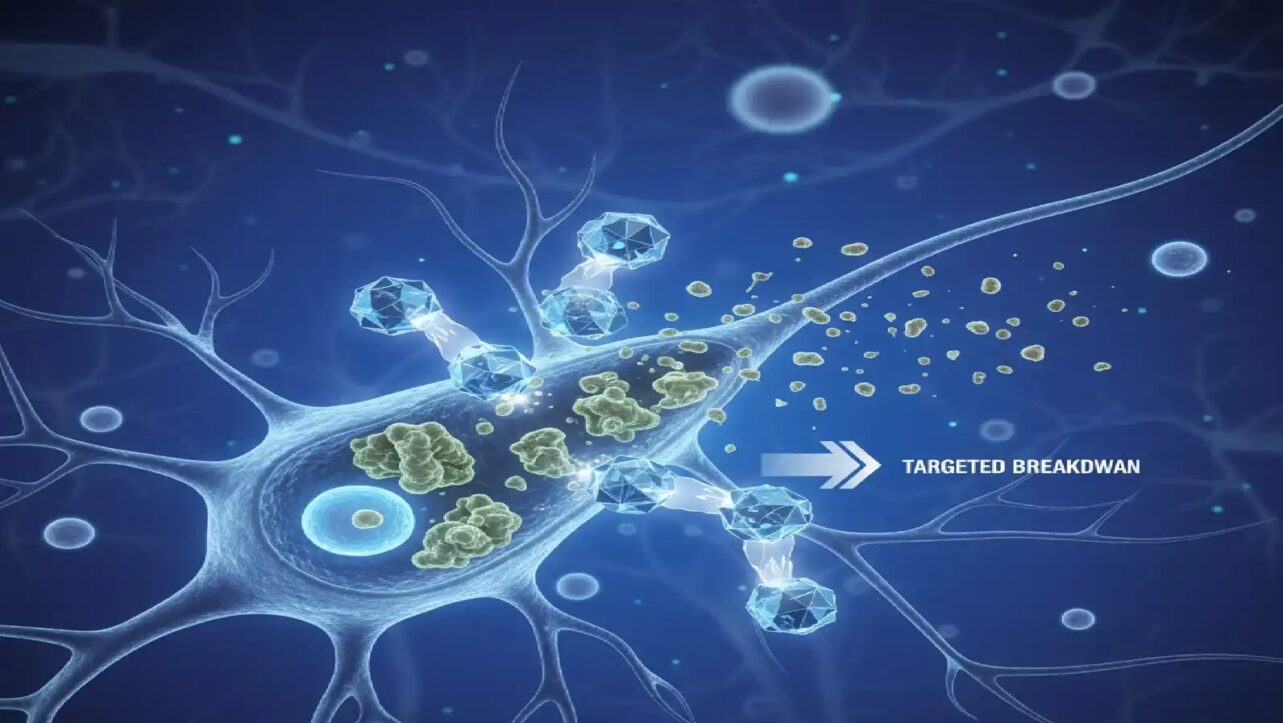
The implant is a 2mm by 2mm photovoltaic chip surgically placed beneath the retina in the region where natural photoreceptors have been lost. Unlike healthy photoreceptors that respond to visible light, this chip detects invisible infrared light projected from a small camera mounted on the smart glasses worn by patients. The camera captures visual information and converts it into infrared signals, which the implant transforms into electrical impulses to stimulate the remaining retinal neurons. This wireless technology is powered solely by light, eliminating the need for external power sources or cables, which were limitations in earlier prosthetic eye designs.
According to Daniel Palanker, PhD, a professor of ophthalmology and co-senior author of the study, “All previous attempts to provide vision with prosthetic devices resulted in basically light sensitivity, not really form vision. We are the first to provide form vision.” Palanker reflected on the invention’s genesis, saying, “The device we imagined in 2005 now works in patients remarkably well.”
What sets PRIMA apart is its ability to enable users to combine their natural peripheral vision with the artificial central vision provided by the implant. This fusion allows patients enhanced orientation and navigation capabilities, something crucial for daily functioning. “The fact that they see simultaneously prosthetic and peripheral vision is important because they can merge and use vision to its fullest,” Palanker explained. The glasses also offer customizable digital enhancements, including adjustable zoom and contrast, enabling users to read books, food labels, and signage with clarity and ease.
While some patients were able to distinguish shapes immediately after activation, the majority experienced gradual improvement over months of training, similar to the adaptation process seen with cochlear implants for hearing restoration. The average patient improved five lines on the eye chart, with one participant showing an unprecedented twelve-line gain in visual acuity. Two-thirds of users reported medium to high satisfaction with the device.
Though some participants experienced mild side effects such as ocular hypertension and peripheral retinal tears, these were non-life-threatening and mostly resolved within two months.
Looking forward, ongoing development efforts focus on enhancing the implant’s capabilities. Currently delivering black-and-white vision without grayscale, researchers are working on software updates to enable the full spectrum of grayscale necessary for finer recognition tasks like face identification. Additionally, Palanker noted, “Number one on the patients’ wish list is reading, but number two, very close behind, is face recognition. And face recognition requires grayscale.”
The team is also engineering next-generation implants with pixels as small as 20 microns—down from 100 microns—potentially increasing resolution more than 25-fold. “This is the first version of the chip, and resolution is relatively low,” Palanker said. “The next generation of the chip, with smaller pixels, will have better resolution and be paired with sleeker-looking glasses.” He added that with smaller pixels and electronic zoom, patients “could get close to 20/20” vision.
The PRIMA project is the fruit of decades of innovation, from initial concept to animal trials and multi-center human studies, involving collaboration among leading academic institutions globally. It offers hope to over five million people worldwide with AMD, whose central vision has been irreversibly damaged. This breakthrough marks a paradigm shift from slowing progression of blindness to actively restoring lost vision and independence.
This transformative technology combines cutting-edge bioengineering, optics, and neurology to redefine possibilities in sight restoration, promising enhanced quality of life for millions affected by degenerative eye diseases worldwide.