A 24-year-old British woman has shared a harrowing warning from her hospital bed after what began as ordinary back pain spiraled into complete paralysis within just seven days, leaving her unable to move, speak clearly, or care for herself.
Kaci Shiers documented her terrifying ordeal on Instagram on October 15, revealing how Guillain-Barré syndrome—a rare neurological disorder—transformed her from a healthy young woman into someone fighting for her life in a matter of days.
“Am I Dying?” – Kaci’s Week From Hell
Shiers’ nightmare began on September 23 when she woke up with back pain she initially dismissed as a pinched nerve. What happened next unfolded with frightening speed.
Within days, she developed leg weakness that caused her to fall down stairs. One side of her face became paralyzed. She lost the ability to walk or move independently. Her bladder stopped functioning.
“Just a week before hospitalization, I was a typical 24-year-old woman, but suddenly I couldn’t wash, feed, or groom myself,” Shiers shared from her hospital bed.
Doctors Didn’t Take Her Seriously at First
Perhaps most alarming was Shiers’ revelation that healthcare professionals initially failed to recognize the severity of her condition when she first sought help. This delay in diagnosis is particularly dangerous given how rapidly Guillain-Barré syndrome can progress from mild symptoms to life-threatening paralysis.
After spending considerable time unconscious in hospital, Shiers recalled asking doctors a haunting question: “Am I dying?”
“I underwent numerous tests – several MRIs, CT scans, and a lumbar puncture, and then my bladder stopped functioning exactly one week into my hospital stay,” she revealed. Doctors have since detected swelling in her brain and spine that is not typically associated with Guillain-Barré syndrome, adding another layer of medical mystery to her case and requiring ongoing investigation.
What Is Guillain-Barré Syndrome?
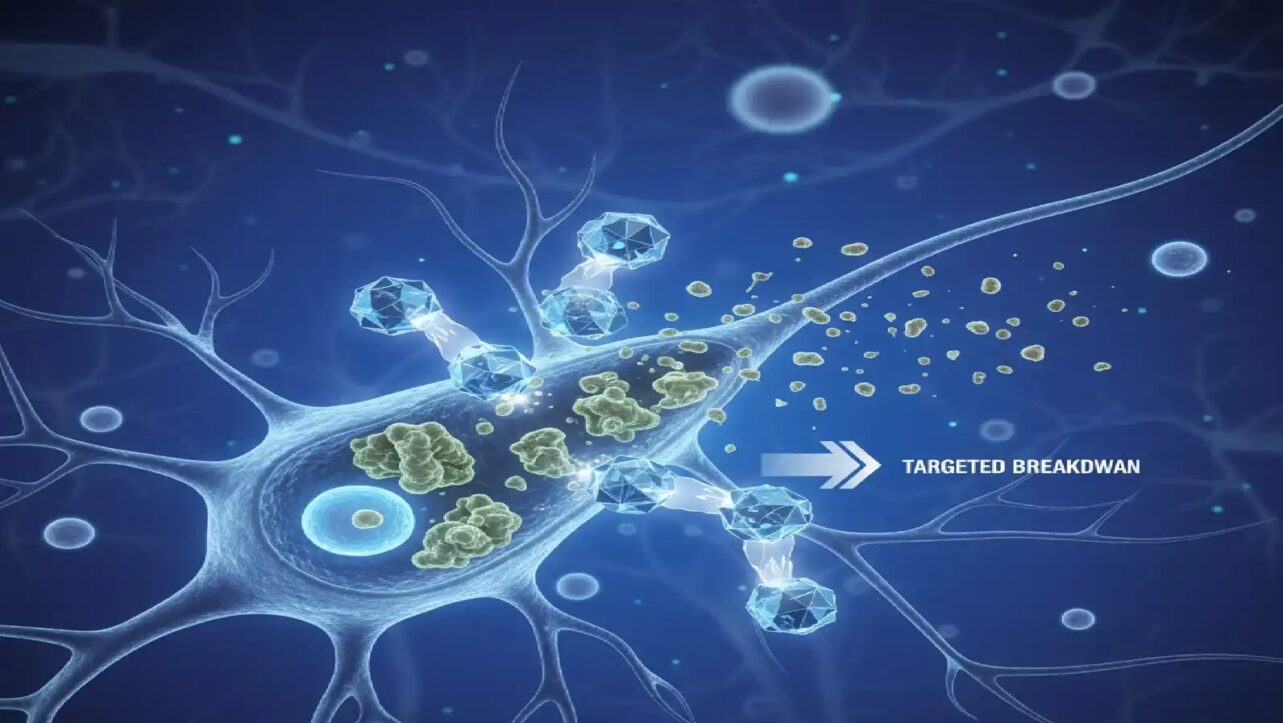
Guillain-Barré syndrome (GBS) is a rare neurological disorder where the body’s immune system mistakenly attacks the peripheral nervous system—the network of nerves outside the brain and spinal cord.
This autoimmune response strips away the protective myelin sheath covering nerve fibers, disrupting nerve signal transmission and causing progressive muscle weakness and paralysis. Symptoms typically start in the legs and progress upward through the body over days to weeks.
In severe cases, paralysis can affect breathing muscles, requiring mechanical ventilation and intensive care. The condition affects approximately 1-2 people per 100,000 annually worldwide, making it rare but not exceptional.
What Causes Guillain-Barré Syndrome?
GBS typically develops following an infection, though the exact mechanism of how infections trigger the autoimmune response remains unclear. The immune system begins attacking healthy nerve cells, mistaking them for invading pathogens.
Most Common Triggers:
- Campylobacter jejuni bacteria – Found in undercooked poultry, this is the single most common GBS trigger, accounting for approximately 30% of all cases. About 1 in every 1,000 people with Campylobacter infection develops GBS.
- Viral infections – Including influenza, COVID-19, cytomegalovirus, Epstein-Barr virus (mononucleosis), and Zika virus.
- Respiratory infections – Upper respiratory tract infections in the weeks preceding paralysis.
- Other bacterial infections – Mycoplasma pneumonia and hepatitis viruses.
- Surgery or trauma – Occasionally triggers the syndrome.
- Vaccinations – Extremely rare, with studies showing people are far more likely to get GBS from infections like flu than from the vaccine preventing those infections.
About two-thirds of people who develop GBS had diarrhea or respiratory symptoms in the days or weeks before neurological symptoms appeared. Recent research investigating the 2025 Pune GBS outbreak identified mutated Norovirus in patients who developed paralysis after gastrointestinal symptoms, adding Norovirus to the growing list of viral triggers. .
The Warning Signs of Guillain-Barré Syndrome
Shiers’ viral Instagram warning focuses on symptoms that are easily dismissed as minor ailments. Her message: these signs should never be ignored when they rapidly worsen.
Critical Early Warning Signs:
- Unexplained back pain or severe muscle aches – Often mistaken for pulled muscles or poor posture
- Tingling sensations in fingers and toes – The “pins and needles” feeling that spreads
- Weakness in legs – Difficulty climbing stairs or standing from sitting
- Recent stomach bug or diarrhea – Gastrointestinal infections in preceding weeks
- Facial changes – Difficulty moving facial muscles, swallowing, or speaking
- Rapid progression – Symptoms worsening over hours to days rather than weeks
When to Seek Emergency Care Immediately
Medical experts emphasize that GBS is a medical emergency requiring immediate hospitalization.
Go to A&E immediately if you experience:
- Rapidly worsening muscle weakness in legs or arms
- Difficulty breathing or shortness of breath
- Severe pain in back, neck, or extremities following an infection
- Loss of bladder or bowel control
- Facial paralysis or difficulty swallowing
- Tingling that spreads quickly upward from feet to torso
Early intervention is crucial. Patients who sought treatment promptly had significantly better outcomes, with many recovering within weeks compared to months for those with delayed diagnosis.
Treatment and Recovery Prospects
The good news is that most GBS patients experience significant recovery, though the timeline varies widely.
Standard Treatment Includes:
- Intravenous Immunoglobulin (IVIG) – Provides healthy antibodies to block the damaging immune response
- Plasma Exchange (Plasmapheresis) – Removes harmful antibodies from the bloodstream
- Supportive Care – Mechanical ventilation if needed, pain management, bladder catheterization
- Intensive Rehabilitation – Physical and occupational therapy to rebuild strength and function
According to the NHS, most people will regain the ability to walk within six months, with full recovery typically occurring within a year. Approximately 80% of GBS patients regain independent walking ability within six months, though some may experience long-term weakness, fatigue, or neuropathic pain.
Kaci’s Message of Hope
Despite the severity of her condition, Shiers is now documenting her recovery progress on social media, offering hope to others facing similar diagnoses.
“I can now sit up and lift my head,” she shared in recent updates. “With assistance, I’ve managed to stand, something I couldn’t do just two days ago. It’s like taking baby steps, and this recovery will not be swift. It will undoubtedly be the most challenging ordeal of my life“.
She emphasized the emotional reality: “I was just a regular 24-year-old, and now I have to relearn how to walk“.
Kaci expressed heartfelt appreciation for her family and friends who supported her throughout this frightening experience. “It’s been incredibly daunting, but their presence has made it a bit more bearable. I’ve never felt isolated in this situation“.
Her viral warning has resonated with thousands: trust your instincts when something feels wrong, advocate for yourself when healthcare providers dismiss your concerns, and never ignore back pain that rapidly worsens alongside neurological symptoms.
The discovery of norovirus as a GBS trigger underscores an important preventive measure: take stomach infections seriously. Seek medical attention for severe gastroenteritis, practice rigorous hand hygiene, and avoid consuming food or water from questionable sources—especially during travel.
Kaci Shiers’ courage in sharing her story from her hospital bed may save lives by teaching others to recognize the early warning signs that medical professionals sometimes miss. Her message is simple but urgent: when your body is telling you something is seriously wrong, demand to be heard.