A groundbreaking study published on October 23 2025 in Nature Biotechnology is challenging a widely-used fertility treatment that may be unnecessarily discarding healthy embryos, potentially costing couples thousands of dollars and delaying their chances of conception.
Scientists at the University of Cambridge’s Loke Centre for Trophoblast Research have discovered that pre-implantation genetic testing for aneuploidy (PGT-A)—a screening method used in fertility clinics worldwide to assess IVF embryos—likely overestimates the number of embryos with chromosomal abnormalities.
Using revolutionary real-time imaging technology, researchers found that many detected abnormalities occur in cells destined to become the placenta, not the fetus itself, meaning these “flawed” embryos could still develop into healthy babies.
The High-Stakes Test Under Scrutiny
PGT-A testing is commonly offered as a treatment “add-on” to older women and those with a history of recurrent miscarriages or multiple IVF failures. The test screens embryos before implantation by taking cell samples from the outer layer of the blastocyst—the hollow ball of cells formed about six days after fertilization.
When chromosomal abnormalities are detected, embryos are often deemed inviable and discarded, forcing patients to undergo another expensive and emotionally draining treatment cycle. However, this new research suggests that some of those discarded embryos may have been perfectly capable of developing into healthy pregnancies.
“Having a baby through assisted conception can be very challenging,” said Professor Kathy Niakan, Director of the Loke Centre for Trophoblast Research and Co-Chair of Cambridge Reproduction. “Most embryos fail to develop or to implant, and even those that are good quality may not be transferred. Much more basic research is needed to inform future clinical practice and improve rates of assisted conception.“
Revolutionary Imaging Reveals Hidden Truth
To understand what happens during the earliest stages of embryo development, Professor Niakan’s team, in collaboration with the Francis Crick Institute, developed a cutting-edge imaging method that allows scientists to watch embryos develop in real-time without damaging them.
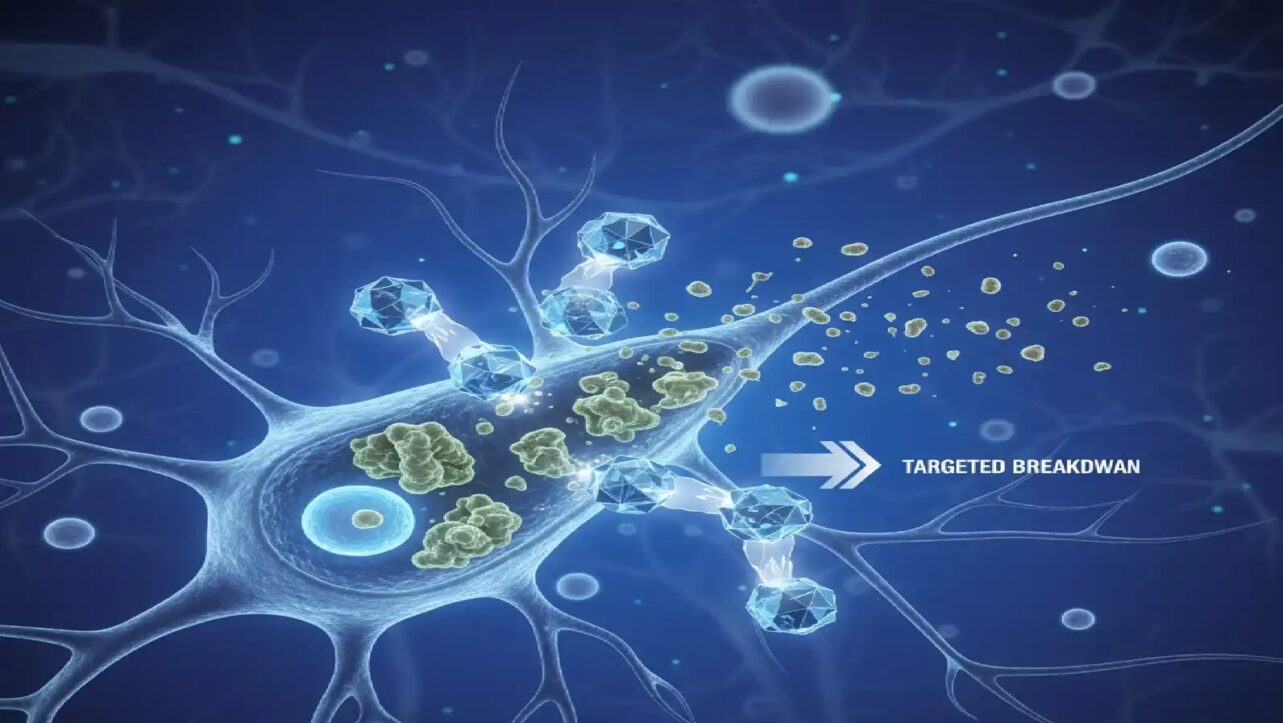
The technique uses fluorescent tagging to mark DNA inside cell nuclei, combined with light-sheet microscopy to observe embryos in 3D as they divide and grow. This gentle yet high-resolution approach permitted continuous monitoring over two-day intervals, capturing rare cellular events that were previously invisible.
First author Dr. Ahmed Abdelbaki, a postdoctoral researcher at the Loke Centre, said: “This is the first time that this very gentle method, with much higher resolution, has been used. It meant that we could watch the embryos as they developed over a two-day period, the longest continuous time that this process has been observed“.
Co-author Professor Ben Steventon from the Department of Genetics at the University of Cambridge added: “The unique design of the microscope allows for multiple precious embryos to be watched simultaneously, and from both sides. This has allowed the team to catch events that have previously been missed. It’s a proof of the power of direct observation to uncover unexpected findings in human biology“.
The Unexpected Discovery
During their investigation, researchers monitored 13 embryos donated by families with successful pregnancy histories and discovered that approximately 10% of observed cells presented chromosomal irregularities. These abnormalities arose from problems when DNA is being copied between cells, such as when chromosomes did not move properly during division or when a cell divides into three rather than two.
Professor Niakan, the study’s senior author, said: “We were extremely surprised to discover that abnormal cell divisions can happen from scratch at a very late stage of human development. It was only by using a new imaging technique that it was possible to see this happening“.
Why Location Matters
The timing and location of these chromosomal errors are critical to understanding embryo viability. The study revealed that abnormalities arise at a relatively late stage of embryo development and appear specifically in the outer layer of the blastocyst.
Because PGT-A testing takes biopsies from this outer layer to assess the entire embryo’s health, the test may be detecting problems that would only affect the placenta—a temporary organ that supports the pregnancy but isn’t part of the baby itself.
“Our research demonstrates that errors in chromosome segregation can occur at comparatively late stages, specifically within the trophoblast—the precursor to the placenta—rather than within the inner cell mass that leads to the fetus,” Professor Niakan explained. “This challenges the assumption that all detected aneuploidies are detrimental to embryo viability.“
Critical Research Still Pending
Crucially, Professor Niakan’s team has not yet studied the inner cell mass—the cells that actually develop into the fetus—to determine whether these late-stage abnormalities also arise there. This investigation is now underway and will be essential for determining the full implications of the findings.
If the inner cell mass remains chromosomally normal while the outer layer develops abnormalities, it would confirm that current PGT-A practices may be unnecessarily discarding viable embryos. However, until this research is completed, the full clinical significance remains uncertain.
The Cost of Uncertainty
Infertility affects millions of couples globally, with assisted reproductive technology demand rising steadily. In assisted conception procedures, as many as nine in ten embryos fail to develop to a stage where they can be transferred to the womb.
The financial and emotional toll is substantial. Each IVF cycle can cost tens of thousands of dollars, and when embryos are discarded based on PGT-A results, couples must restart the grueling process—hormone injections, egg retrieval, fertilization, and the agonizing wait.
If the test is indeed overestimating abnormalities and leading to the disposal of viable embryos, it could be significantly reducing success rates while increasing the time, cost, and psychological burden on already vulnerable patients.
Global Implications for Fertility Treatment
This research has profound implications for fertility clinics worldwide, including India’s rapidly growing IVF industry. India has emerged as a major destination for fertility treatments, with hundreds of clinics offering PGT-A testing as a premium service to improve success rates.
The findings call for an urgent reassessment of current PGT-A practices and advocate for new techniques that can distinguish between placental and embryonic genetic abnormalities. Such precision could revolutionize embryo selection, improve IVF success rates, and significantly reduce unnecessary treatments and patient distress.
Technical Breakthrough Opens New Possibilities
The study represents a significant technical leap in reproductive biology, opening unprecedented windows into human embryogenesis—knowledge that is crucial for unraveling the origins of developmental disorders and improving assisted conception outcomes.
The embryos used in this study were donated by families who had successful pregnancies at Bourn Hall Clinic and Create Fertility. The research was supported by Wellcome, the Francis Crick Institute (which receives core funding from Cancer Research UK, the Medical Research Council and Wellcome), and the Engineering and Physical Sciences Research Council.
The study underscores the remarkable adaptability and resilience of early human embryos. While chromosomal errors in trophoblast cells may not doom an embryo, their presence could still affect placental function and pregnancy outcomes—a nuance that current genetic tests fail to capture.